
UMDAA PROTOCOL FOR COVID - 19
Post By: Dr. Abdul Khaliq
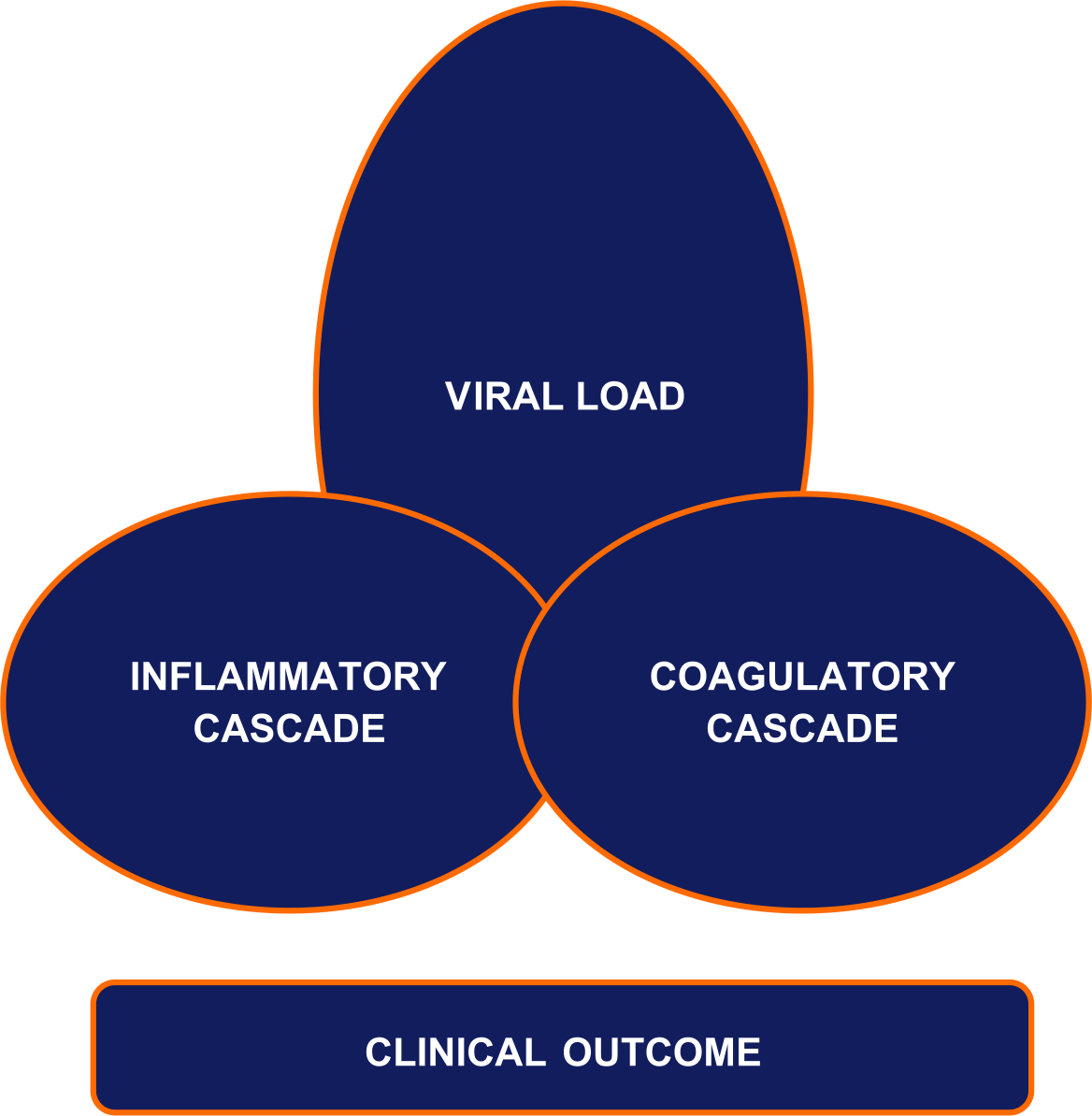
Pathophysiology:
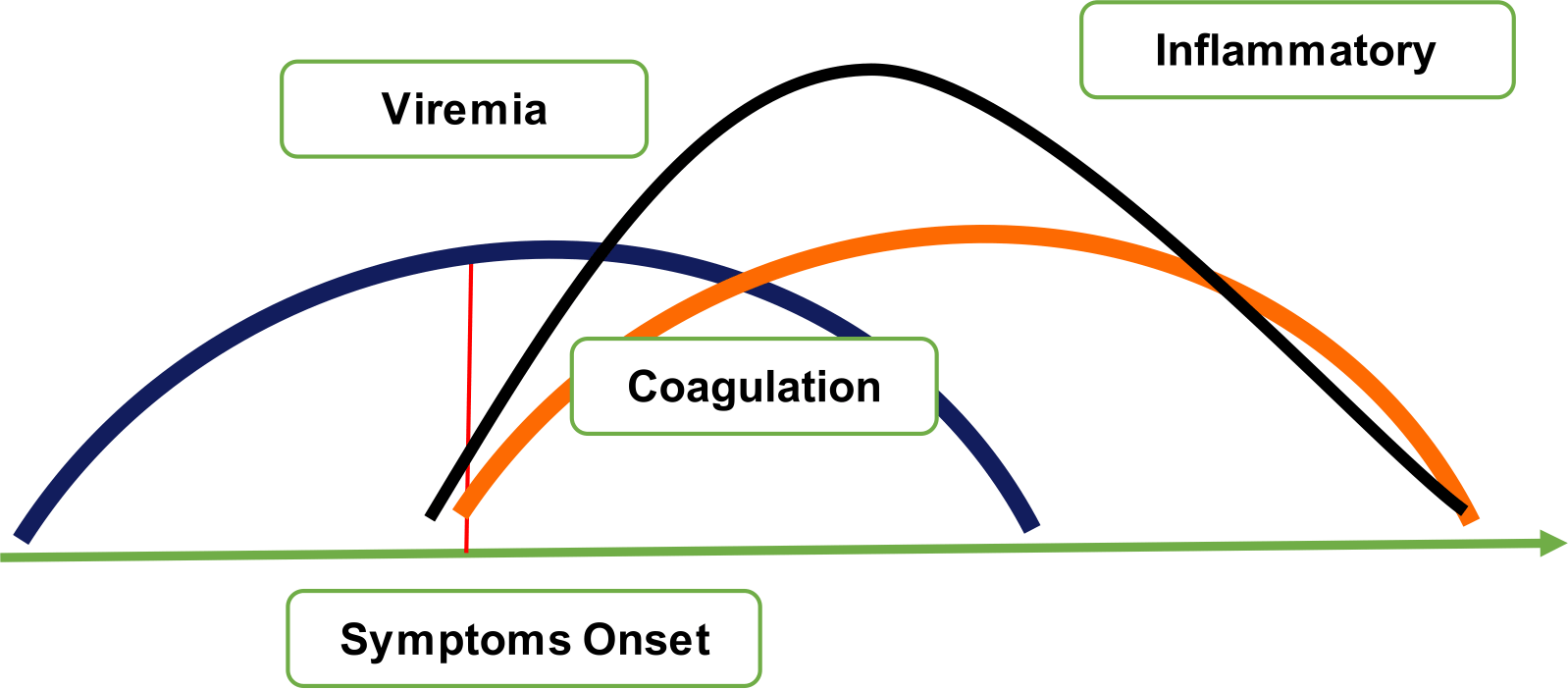
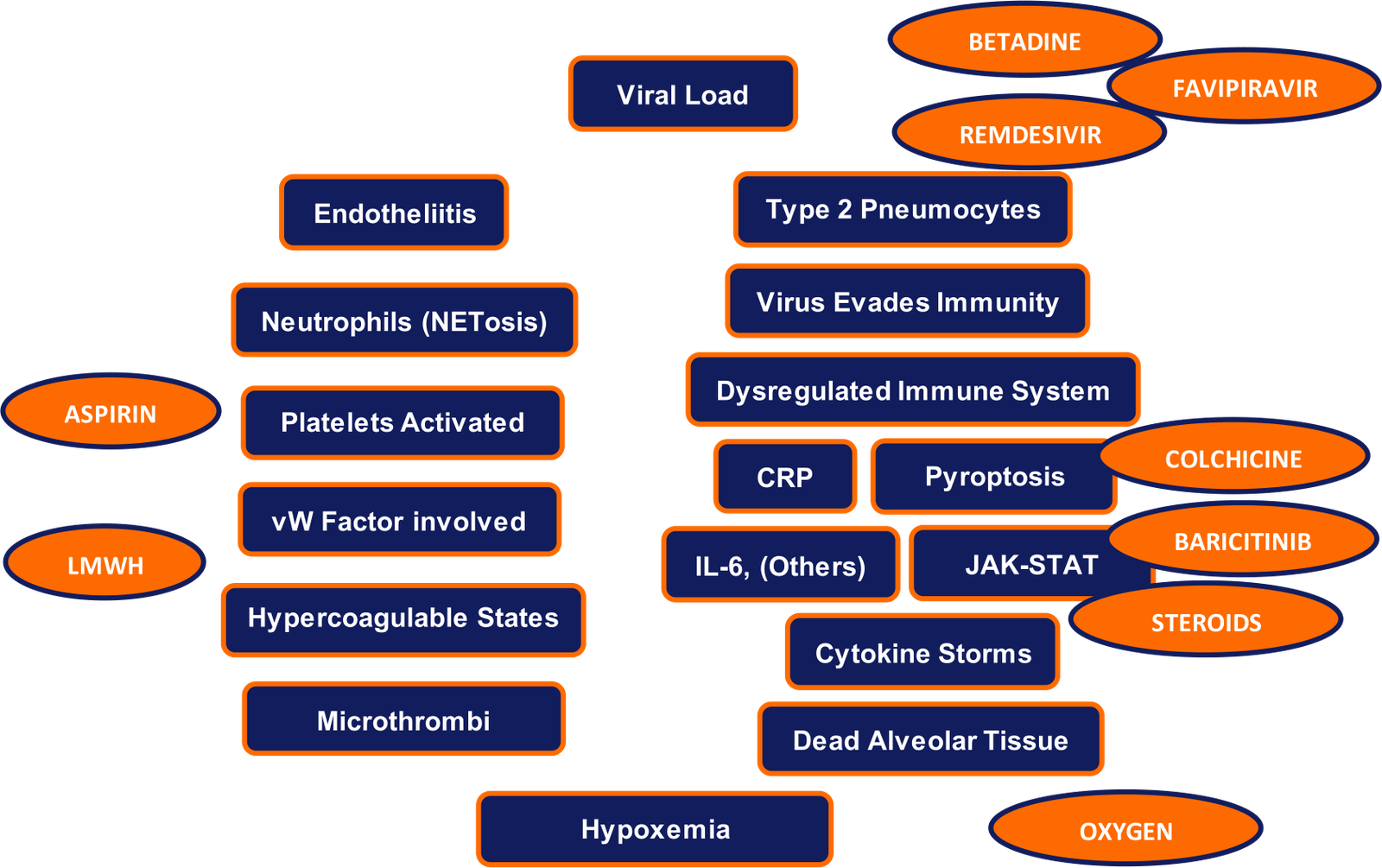
Pathogenesis:

Drugs: Mechanism of action
Categorization of Patients:
|
Groups |
Group A |
GROUP B |
GROUP C |
|
Definition |
Potential for good outcome |
Group A bit worsens into group C |
Potential for poor outcome |
|
Demographics |
Age < 45 No obesity No comorbidities ? Completed full vaccination |
|
Age > 45 Obesity Co-Morbidities Pregnancy Immunosuppressive Medications |
|
Symptoms |
Any Symptom |
Persistent high grade fever (> 101F) for more than 5 days Severe Myalgia’s Severe fatigue |
Any symptoms |
|
Labs |
|
ALC < 1000 Eosinophils – 0 NLR > 3.2 D-dimer > 1.0 LDH > 250 Ferritin 300-800 CRP 15-40
|
ALC < 80 CRP > 40 CRP increase more than 10 in 3 days LDH > 500 Ferritin > 800 NLR > 3.2 D- Dimer > 1.5(3 n) |
|
CT Scan |
|
30% - 50% involved |
> 50% involved |
|
Treatment |
Betadine Steam Inhalation
Famotidine Colchicine Aspirin Multivitamins |
+ Favipiravir / Remdesivir
+LM WH / Oral Anticoagulants
|
+ Remdesivir + LM WH / Oral Anticoagulants
|
|
6 minutes’ walk Hypoxemia |
Less likely to have Hypoxemia |
Baricitinib / Steroids |
Baricitinib / Steroids |
Management According to Groups:
|
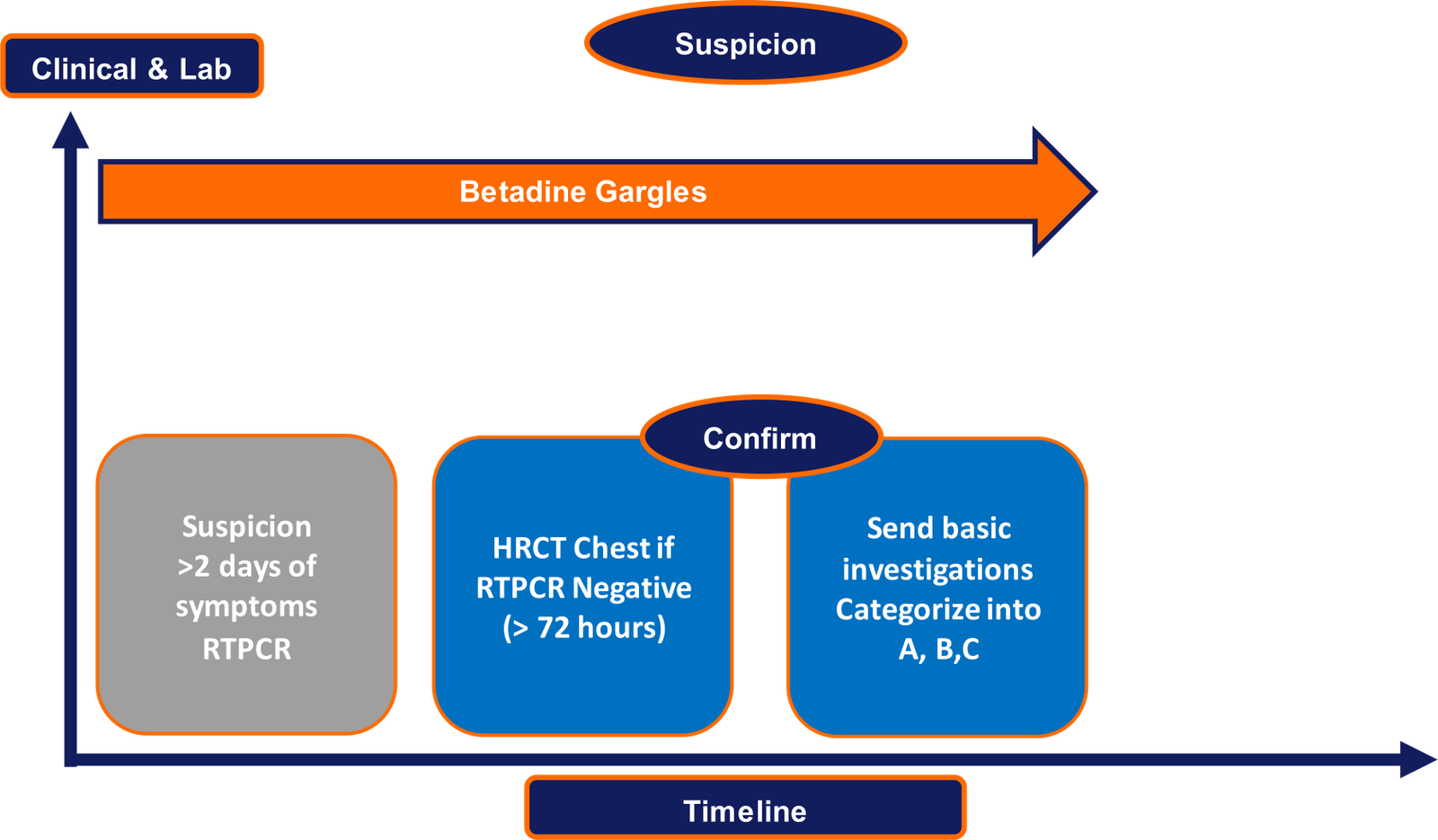
Suspicion |
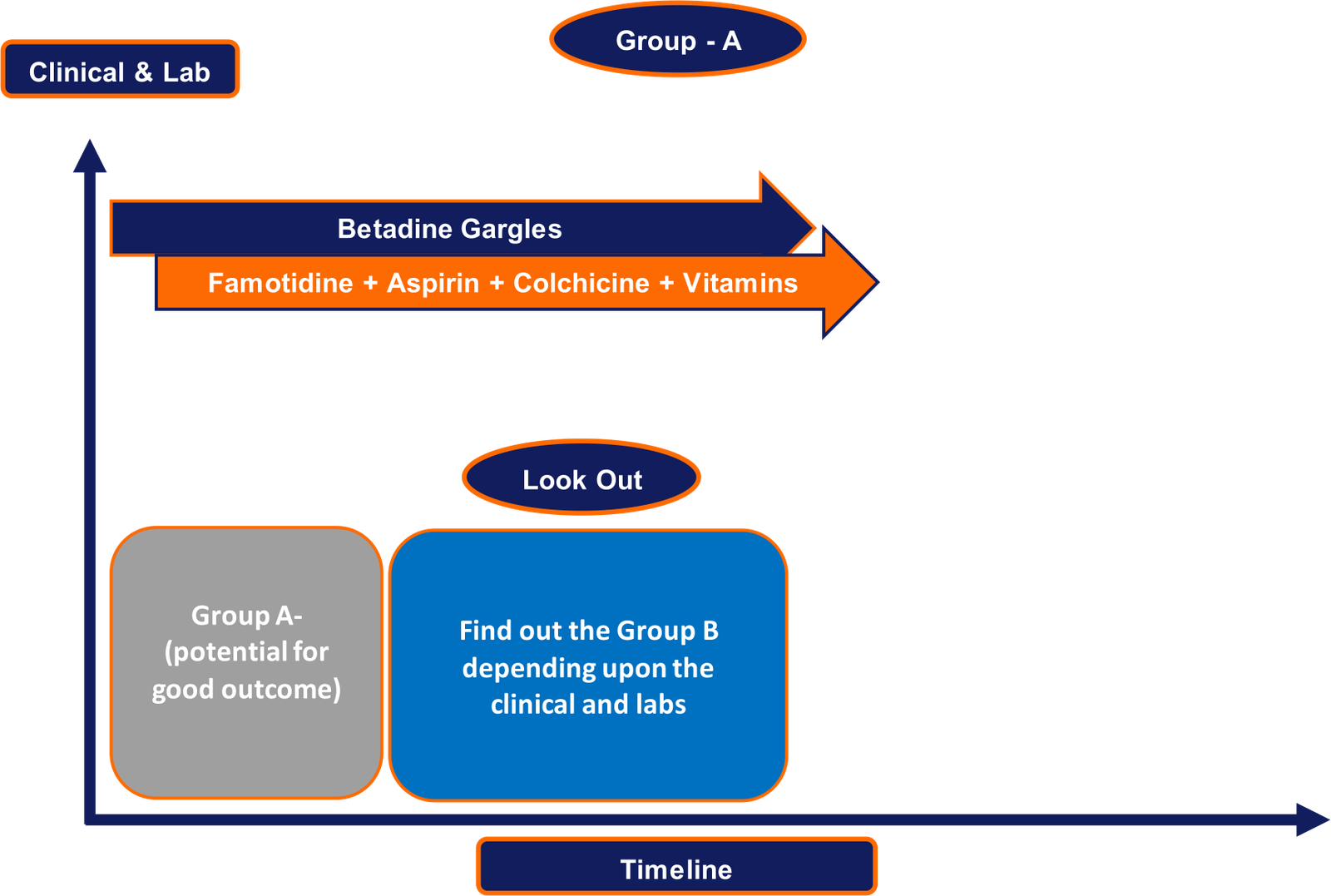
Group – A |
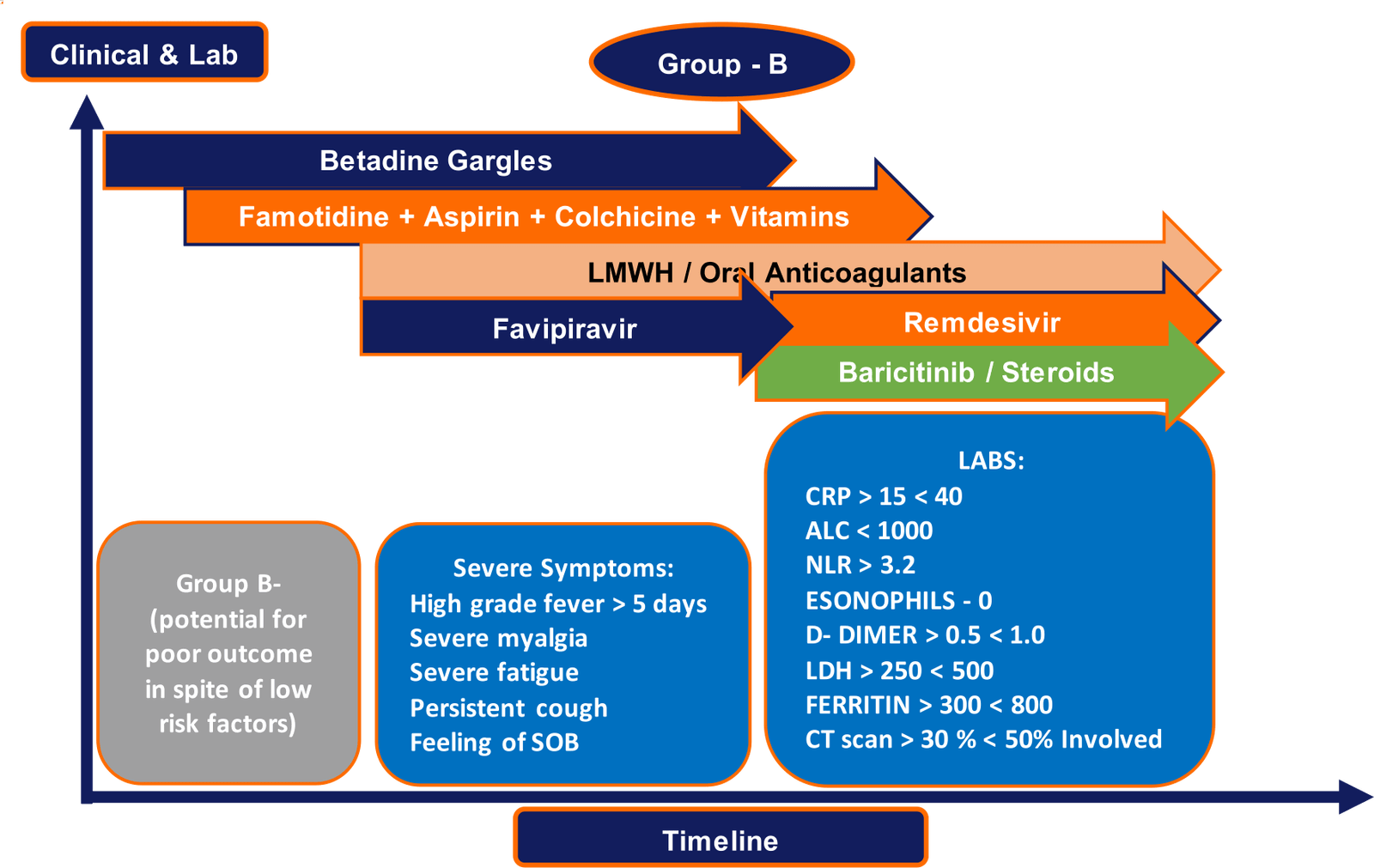
Group – B |
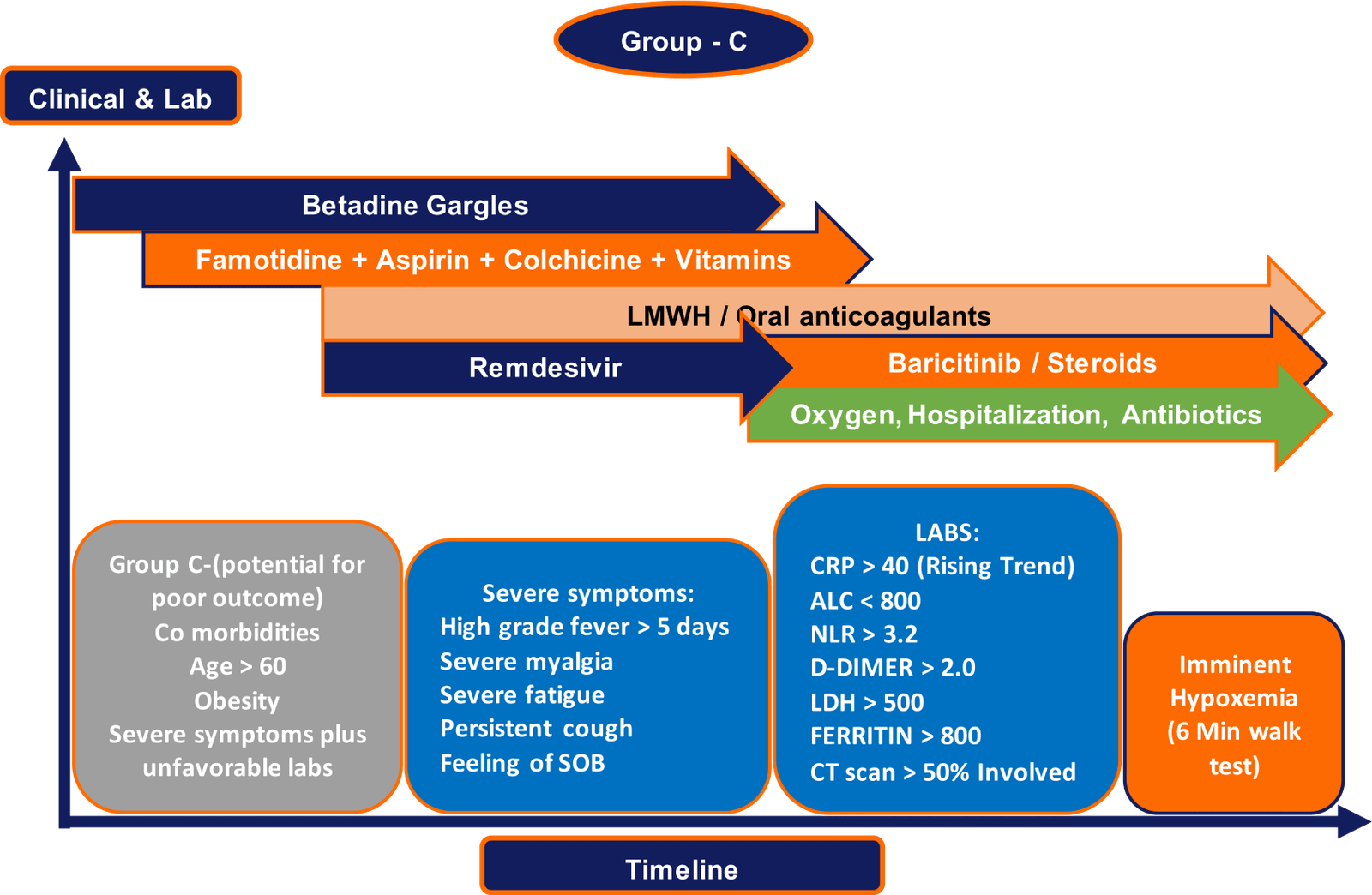
Group – C |
|
Betadine Steam inhalation |
Famotidine: 40 mg BD before breakfast 5-10 days
Aspirin: 75 mg post lunch. 5-10 days
Colchicine: 0.5 mg BD for 3 days f/b OD after food for 5-10 days
Zincovit: OD after lunch for 5-10 days
Vitamin D: 60k stat |
Famotidine: 40 mg BD before breakfast 5-10 days
Aspirin: 75 mg post lunch. 5-10 days
Colchicine: 0.5 mg BD for 3 days f/b OD after food for 5-10 days
Zincovit: OD after lunch for 5-10 days
Vitamin D: 60k stat
LM WH(Enoxaparin): 40 -60 mg s/c OD-BD
Favipiravir: 1800 mg BD for day 1 followed by 800 mg BD for 7-14 days
Remdesivir: 200 mg followed by 100 mg for 5 days (slow iv)
Baricitinib: 4 mg/day for 14 days
Steroids: dexamethasone 6 mg/d
|
Famotidine: 40 mg BD before breakfast 5-10 days
Aspirin: 75 mg post lunch. 5-10 days
Colchicine: 0.5 mg BD for 3 days f/b OD after food for 5-10 days
Zincovit: OD after lunch for 5-10 days
Vitamin D: 60k stat
LM WH(Enoxaparin): 40 -60 mg s/c OD-BD
Remdesivir: 200 mg followed by 100 mg for 5 days (slow iv)
Baricitinib: 4 mg/day for 14 days
Steroids: dexamethasone 6 mg/d
|
Colchicine 0.5 mg up to even thrice daily for 5 days is the maximum. Maintenance can be 0.5 mg BD up to another 5 days.
Dexamethasone6 mg is equivalent to 40 mg of prednisolone, 32 mg of methyl prednisolone and160 mg of hydrocortisone.
Caution of medications:
Colchicine:
Be aware of interaction with Statins if patient is already on particularly in elderly with renal dysfunction. It may cause myalgia’s and myolysis.
Avoid concomitant use with azithromycin- QT interval changes
Be cautious if renal dysfunction and cirrhosis
Avoid in pregnancy and lactation.
Diarrhea, muscle pain, nausea vomiting and abdominal pain can occur.
Aspirin:
Gastritis, UGI Bleed, worsening renal function
Baricitinib:
Avoid in pregnancy and lactation
Cytopenia scan occur
Add antibiotic cover as it reduces immune response
Q & A:
- When should the patient get tested and what tests?
- Can the patient get Rapid antigen test?
- What should the patient do when waiting for the reports?
- Isolate
- Betadine gargles
- Steam inhalation
- How to use Betadine Gargles?
- How to use steam inhalation?
- What to do if Clinical symptoms are like COVID-19 but RT PCR is negative?
- If HR CT is noncontributory in RT PCR Negative case then what?
- What are the medications to start with if in Group A?
- Most of the patients in group A will improve with good outcome. Baseline supportive medications and symptomatic medications are required.
- Supportive medications : Famotidine, aspirin, statin, colchicine, zincovit, vitamin D sachet
- Symptomatic medications: paracetamol, ascoril, cetirizine, etc.
- When are tests required in Group A?
- At baseline and repeat at 3-5 days if severe symptoms persisting (fever/myalgia/fatigue/cough/sob) or when labs are abnormal as described.
- At baseline and repeat at 5-7 days if mild symptoms persisting and mild derangement in labs
- At baseline and need not repeat if symptomatic improvement and all lab parameters within normal.
- How to identify Group B from amongst Group A?
- Severe symptoms (High grade fever>101F, Myalgia’s, undue fatigue, persistent cough, dyspnea) persisting more than 5 days
- Lab parameters as described in table (at least 1 lab parameter abnormal). High reliance is given to CRP, NLR and D-dimer.
- When to start antivirals in Group B and which antivirals?
- Once identified as Group B give antivirals
- Favipiravir if mild elevations in labs /symptoms persisting
- Remdesivir if significant elevation in lab as in group C / CT > 50% involvement
- If started on Favipiravir of group B then when to shift to remdesivir?
- Can Remdesivir be started in Group B right at the onset of inflammatory cascade?
- What medications to start in group C?
- Group C are either age more than 45,obesity, co-morbidities then
- Betadine, steam inhalations
- Famotidine, aspirin+ statin, colchicine, multivitamins, Vitamin-D
- LM WH right at onset 40- 60 mg depending upon age
- Remdesivir under medical supervision.
- When to retest for labs in group C/ group B?
- What if labs are worsening along with clinical status co or worsening in Group C/ B in spite of Rem, LM WH?
- If D-dimer is increasing consider optimizing LM WH to therapeutic dose or twice a day 60 mg
- If CRP/ Ferritin / NLR is worsened along with clinical worsening consider optimizing colchicine or add on Baricitinib if within 1 week and no hypoxemia on 6-min walk test.
- If still CRP/ Ferritin/NLR is worsening along with clinical worsening in spite of adding colchicine and Baricitinib -consider getting HR CT for lung involvement- if it is > 40% involved consider adding steroids in spite of no hypoxemia.
If symptoms persist for more than 2 days go ahead and get the RT PCR done. The reason for early testing is if early diagnosis is made then early treatment and better prognosis is anticipated. More or less because of increasing cases sometimes getting report is not possible on the same day in multiple places. So the dictum is early the testing done the better for management.
Rapid antigen testing can be done but if the report is available immediately. Once a rapid antigen test is negative, RT PCR has to be tested again. If getting report is delayed better to go ahead with the standard of the testing that is RT PCR.
Betadine gargles protocol 15 ml twice a day for 1 minute 1% povidine iodine. Dilute 10% Betadine 2 ml with 20 ml of water. Rinse through both nostrils and gargle through mouth for at least 1minute twice a day. For 5 days to 7 days. (Oral This. 2020.10.1111/odi.13526d).
Steam inhalation protocol: Each session of 4 minutes - total 5 sessions (that is 20minutes of total exposure) with in 1-hour period. Heat denatures the virus mainly in the paranasal sinuses. For 5 days to 7 days (doi.org/10.1016/j.lfs.2020.118801).
In such a case it is better to go ahead with HR CT chest after at least 3 days of symptom onset. It is more likely to help in diagnosing with presence of classical radiological findings.
Then look for other causes depending upon the symptoms. If clinical suspicion is high wait for 2 days more and get RT PCR again.
(Baseline good characteristics but outcome will be poor if unattended early)
Though no enough data but Remdesivir is perceived to be better. So in spite of Favipiravir if repeat markers are showing worsening in the labs done after 2-3 days better to change to Remdesivir
Yes, Remdesivir can be started right at the beginning subject to availability and given under healthcare observation.
All labs or preferably CBP, CRP to be repeated after 3 days.